Child Tonsillectomy Recovery – A Day by Day Guide to Eating, Drinking and Healing from Surgery
Child Tonsillectomy Recovery
Child tonsillectomy recovery doesn’t have to be so bad! I’ll share how our family survived the first 14 days following this major surgery. Our three year old required this procedure to improve many aspects of her health. I’ll share our family’s day by day experience with child tonsillectomy recovery.
If your little one is scheduled to have a tonsillectomy, I have a little idea of how you might be feeling. I felt nervous, excited, curious, scared, and ultimately ready for the process to begin. After all, it was a life-changing procedure that couldn’t come soon enough for our 3 year old!
She had 100% blockage of her adenoids and enlarged tonsils, making breathing (especially at night) very difficult. I watch videos now of that time and am amazed at how stuffed up she sounded all the time.
This surgery was a life-changer!
As you prepare for the big day (and ultimately the big 2 weeks of child tonsillectomy recovery), here’s our family’s experience. Hopefully this can shed a little light on what we experienced and how we weathered our little one’s tonsillectomy recovery.
More Helpful Resources
Day 1 of our Tonsillectomy Recovery
It was surgery time. Our family felt as prepared as possible. We had all of our documents ready for check-in, a well-prepared hospital bag, and home was ready for recovery. (Check out this Parent Toolkit if you’re looking for help preparing, too.)
We waited patiently in the hospital’s Recovery Room for our daughter. The team of doctors were very communicative with nurses, who kept us posted on the surgery progress.
I’m so thankful for the team’s professionalism and care. We were in good hands (and you will be, too!).
The moment came when she exited the OR and was on her way to the Recovery Room. My first memory is this: I was amazed to see my little one post-surgery. This was my first moment of joy, exhilaration, and confirmation that this surgery was the right choice for our family.
You see, she could actually breathe through her NOSE!
Our little one had 100% blockage from her adenoids, and their removal during surgery made her able to use her nose for the first time in ages.
However, still groggy from a heavy dose of anesthesia, she was definitely not herself for about 2 hours post-op. The fact that she wasn’t even interested in a popsicle was a clear giveaway. She was…uncomfortable…that’s the only way to describe it.
In her initial waking moments she cried, seemed disoriented, and was hard to console. The room was unfamiliar and so were the nurses. We focused on keeping her comfortable and she quickly fell back to sleep.
She seemed unsure why swallowing was so hard, and unsure of what just happened. But Day 1 of our tonsillectomy recovery was probably the hardest on us, not her.
In the 2-3 hours after being wheeled out of the operating room, she faded in and out of sleep. On her final wake, she was clearly more “herself” than during those groggy drifts in and out of sleep.
The Wonderful Nurses
I can’t thank our nursing team enough. This incredible group of people were attentive and reassuring. They helped keep me calm with their care for our daughter.
To all the nurses reading this – thank you for what you do! You made the experience so much smoother for our family, and I’m very grateful.
Home at Last
In total, our entire hospital stay was approximately 7 hours.
Once home, we launched into the prescribed pain management system – our doctor mapped out exactly what we should do, hour by hour. We stuck close to their instructions. We then launched into our “keep her comfortable!” plan: snuggles, movies, and lots of yummy liquids.
What made Day 1 so manageable for us was that she had an instant change physically. For a girl who couldn’t use her nose to breathe (surgeon said 100% blockage by adenoids), seeing her breathe through her nose was like a miracle for us. Worth. It.
Time for the “Get Well Bin”
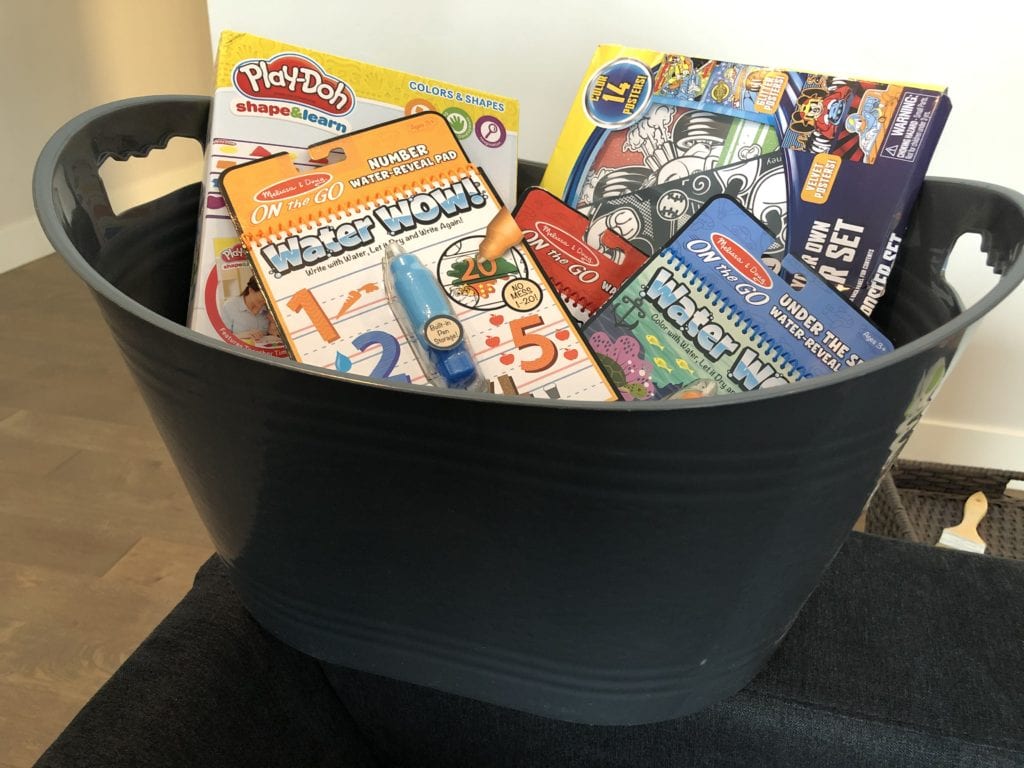
As we prepared for the surgery, we created a “Get Well Bin” (read all about it here!). This was waiting for our daughter in the TV room where we created post-surgery home base.
However, she wasn’t interested in anything in the bin when she got home. Instead, she clearly wanted to rest. We curled up with some Netflix and settled in for a relaxing afternoon.
Cool Mist Humidifier – a MUST!
We took great care (before the surgery) to prepare our home for that moment of arrival. One of the best purchases we made preparing for the surgery was a Pure Enrichment MistAire cool mist humidifier. We started the humidifier the morning before we left for surgery and ran it (non-stop) for two weeks.
The humidifier doesn’t heat up the room and make it humid and uncomfortable; instead it adds moisture to the air. I’m simply speculating here, but I believe the moisture help keep the scars inside from drying out tremendously, especially while sleeping. We filled our humidifier with plain distilled water and ran it on medium low throughout the two-week child tonsillectomy recovery period. Bonus – we’ve since used it dozens of times when anyone in the family gets sick, so it was definitely money well spent.